By Kristin Bundy
Kristin Bundy is a freelance science journalist, reporting here for Scroll Studios. Her work regularly appears in publications, such as MedPage Today and Cancer Therapy Advisor.
Intro
Scroll

Scroll

Scroll


01
Peeling back the layers
02
Mutations and pathways
03
Finding Myelofibrosis
04
Moving beyond
05
What's next

That was the late aughts when the first JAK1/2 inhibitor was in phase 3 studies. Since then, physicians have relied on this drug class to help improve many patients’ lives, says Dr. Mascarenhas, but more needs to be done.
“We don’t see bone marrow fibrosis resolution; we don’t see molecular responses. There are still patients with low platelets and transfusion dependence who are not being served optimally.”
These cases—patients with cytopenias who are challenged by the myelosuppressive nature of current management options—are what motivate Dr. Mascarenhas and his research. He and others have devoted their efforts to address this disparity in MF management.
And he believes we are on the cusp of a new paradigm in MF.
Scroll


Hematologists intrinsically know there are differences in biology and clinical presentation among patients with MF, says Dr. Mascarenhas.
“We do consider platelet count and significant transfusion-dependent anemia. Problem is, right now, we are trying to manage a heterogeneous disease in a homogeneous way.” — John Mascarenhas, MD
For the better part of the last two decades, Dr. Mascarenhas has interrogated the heterogeneity of MF and the inherent differences in pathophysiology between the two types—primary MF (PMF) and secondary MF (SMF). He and other researchers suggest that biological differences between the two may explain why patients respond differently to current management options.
One of the key biological distinctions between PMF and SMF is antecedent disease—SMF is associated with presence of polycythemia vera or essential thrombocythemia while PMF is de novo.
Emerging data show two critical variations between the two phenotypes are mutation profile and the frequency of JAK2V617F allele burden. PMF has a lower JAK2V617F allele burden but more driver mutations; whereas, SMF has a high JAK2V617F allele burden and is associated with just the single mutation.
In the clinic, patients with PMF are more likely to have low blood counts, be transfusion dependent, and have more aggressive disease, while those with SMF are more likely to have myeloproliferation and smoldering disease. Prevalence is different, too.
PMF represents 70% of all MF cases compared with SMF at about 30%.
“Of course, all of these factors appear on a spectrum, not every patient fits perfectly into one or the other, but generally speaking, there does seem to be this dichotomy between primary and secondary MF,” says Dr Mascarenhas.
Unfortunately for patients with MF, physicians have not had a reason to discriminate between the two phenotypes. “Disease management has been pretty uniform for the past decade,” Dr. Mascarenhas explains, and current options can exacerbate cytopenias, forcing dose reductions and limiting clinical benefit. “There's really an unmet need among patients with cytopenias, namely, to improve their low blood counts.”

Patient Story
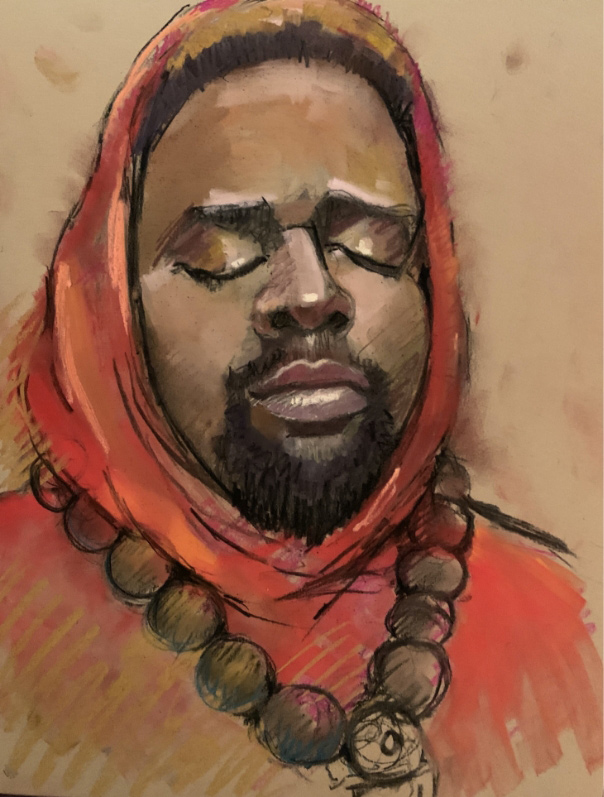
Meet Gail: An artist, teacher, and patient with MF
View Part 1


When Dr. Mascarenhas first started studying MF, little was known about mutations. That changed in 2005, he says, when the JAK2 mutation was discovered. “That revolutionized the way we look at MF and how we classify patients based on the presence or absence of the mutation.” Soon thereafter, mutations on the MPL gene and then the CALR gene were discovered. With three mutations in play, that also meant some patients would be triple negative.
Along with driver mutations, researchers believe variations in allele burden and multiple inflammation-mediated pathways likely drive disease. The latest data show that lower JAK2V617F allele burden portends a worse prognosis and indicates there may be other pathways, outside JAK-STAT, involved in pathogenesis.
“The take home message is there is not going to be one way to manage MF, especially given multiple mutations, variations in JAK2V617F allele frequencies, and multiple potential pathways,” explains Dr. Mascarenhas. “Each is relevant in different ways to different subgroups of patients.”

Patient Story
Overcoming the fear of blood transfusions
View Part 2


As researchers accumulate more knowledge about mutations, allele burden, and pathways that contribute to the heterogeneity of MF, it is also critical to consider the myriad clinical presentations that can play a role in a delayed diagnosis or misdiagnosis, says Dr. Mascarenhas.
Referring physicians and community hematologists may not be as familiar with MF because of the rarity of the disease. And given how many symptoms mimic other conditions (eg, fatigue, early satiety, weight loss, and night sweats), patients with MF inevitably visit several specialists before a hematologist.
“It is not uncommon that I meet patients who have seen cardiologists or pulmonologists for issues related to shortness of breath,” says Dr. Mascarenhas. “I've met patients through gastroenterologists because of bowel irregularity or left upper quadrant pain, which turned out to be splenomegaly. And a common phenomenon is seeing patients after innumerable neurologist consults for headaches or other neurologic symptoms.”
“When we look at things differently and start to realize that there may be
benefits—not just by chance, but mechanistically—to defining different
phenotypes, this can lead to better ways of managing the disease.”
— John
Mascarenhas, MD

It can take months, and sometimes years, for patients to cycle through specialists until patient complaints and abnormal blood counts finally spur a referral to a hematologist.

Patient Story
Staying Connected to Her Art
View Part 3

“I’d like to get that referral earlier,” says Dr. Mascarenhas, “to ensure patients get the care they need.”
By reclassifying and reorganizing the potential mechanistic differences between PMF and SMF, he believes the implications from his research will translate to quicker diagnoses in the clinic.

Being able to manage patients with PMF is a huge unmet need, but what’s encouraging is that some of the infrastructure is in place to rethink the disease, says Dr. Mascarenhas. For example, clinical guidelines already incorporate some of the factors that differentiate PMF from SMF.
“Tucked into the prognostic risk stratification are clinical variables, platelet counts, cytogenetics, and molecular barriers for PMF,” notes Dr. Mascarenhas. “From early on, every prognostic tool included anemia and transfusion-dependent anemia as core prognostic markers.”
For Dr. Mascarenhas, the story of MF having different biologies and different phenotypes has always been there, the community might just need to look at it differently or call it by a different name.
Back in the lab, Dr. Mascarenhas and other researchers are looking to answer some big questions around PMF:

“We want to extend patients' lives. We want them to maintain a good quality of life.” — John Mascarenhas, MD
While the current clinical focus of reducing spleens is important, researchers are taking a holistic view of MF and its many facets, with an eye to modifying the disease process and the disease course. “As we learn more about the biology, we can better understand the differences in MF heterogeneity—which pathways are more relevant in which areas and which should be targeted.”
Dr. Mascarenhas anticipates that the research will bring to bear a shift in how hematologists manage patients with PMF—there will no longer be a one-size-fits-all approach.

Patient Story
Gail's Hope for Tomorrow
View Part 4


01
Peeling back the layers
02
Mutations and pathways
03
Finding Myelofibrosis
04
Moving beyond
05
What's next

Dr. Mascarenhas has hope for the future. “What drives me to work every day is the fact that we're just on the cusp of taking MF management to the next level.” Soon, Dr. Mascarenhas believes the whole concept of PMF—how it is managed and how it is worked-up—will change drastically; he also foresees dramatic shifts in referral patterns and the clinical approach to this segment of hematology.
“Collectively, I don't think any of us researchers are happy with where we are. We’re happy with where we've come from, but we're really looking to improve upon that.”
“I think we are ready for a second renaissance in the management of patients with PMF—one in which hematologists can address the needs of more of their patients.”
—John Mascarenhas, MD
By Kristin Bundy
Kristin Bundy is a freelance science journalist, reporting here for Scroll Studios. Her work regularly appears in publications, such as MedPage Today and Cancer Therapy Advisor.
To hear more on the science of MF from thought leaders,

Disclaimer text sed posuere consectetur est at lobortis. Cras justo odio, dapibus ac facilisis in, egestas eget quam.
©2021 CTI Biopharma

Return to story
Patient Story | Part 1

Scroll

Gail is an artist, a teacher, and a patient with cytopenic MF. She has been under the care of Dr. Mascarenhas and his team since the end of 2019.
Scroll

Scroll

Every three weeks, her husband drives her 3 hours from their home in Maryland to New York City to get a blood transfusion and go to her appointments.
Scroll

Scroll

“There are days when I think, This is not fun at all, but I feel hopeful that things are going to work out, and I’m going to be back to just my regular self again,” says Gail.
Scroll

- Gail

BACK

NEXT

Return to story
Patient Story | Part 2

Play video
Scroll

Scroll

Gail was scared when she got her first blood transfusion “I had no idea what to expect. I was crying. My daughter was trying to comfort me over the phone. Then they brought in the blood—it was quite dramatic.”
Scroll

Now, though, Gail says she is used to getting her transfusions every three weeks; they are a part of her life. She looks forward to feeling better “for two whole weeks,” but during that last week before the next transfusion, she feels slow and not herself.
Scroll

- Gail

BACK

NEXT

Return to story
Patient Story | Part 3
Scroll


For the better part of her career, Gail shared her artistic gifts as a successful children’s book illustrator, and later as a teacher of art and design.
Scroll

Scroll

She enjoyed instructing students in painting and drawing, but as her condition worsened, she didn’t have the energy to stand in front of the classroom.
Scroll


Luckily, she says, the two art schools accommodated her, and now she teaches asynchronous classes online.
Scroll

For a time, it was the only way she stayed connected with the art world. At points during the past year, Gail says she lost touch with her craft.

Scroll

Scroll

“For a long time, I wasn't able to do any art at all. I just didn’t have the energy. I would walk into my studio and see all my stuff just sitting there waiting to be worked on, and I would think, I don’t know how to draw anymore.”
Scroll


- Gail

BACK

NEXT

Return to story
Patient Story | Part 4

Play video
Scroll

Scroll

Gail says she’s not necessarily looking for a cure, she just wants to feel better.
Scroll

Scroll

- Gail

BACK

NEXT